Invasive Coronary
Many procedures are very effective in treating coronary conditions, allowing patients to live fulfilling lives. Although some procedures require extensive open-heart surgery and recovery time, others are common procedures with minimal downtime. If your doctor finds that an invasive coronary procedure is right for you, consult with him or her about prep that may be necessary, the details of the procedure, the recommended recovery period, and the follow-up processes.
Learn more about specific heart conditions and treatments below.
Cardiac Catheter
Cardiac catheterization (cardiac cath or heart cath) is a procedure to examine how well your heart is working. A thin, hollow tube called a catheter is inserted into a large blood vessel that leads to your heart.
- Cardiac cath is performed to find out if you have disease of the heart muscle, valves or coronary (heart) arteries.
- During the procedure, the pressure and blood flow in your heart can be measured.
- Coronary angiography is done during cardiac catheterization. A contrast dye visible in X-rays is injected through the catheter. X-ray images show the dye as it flows through the heart arteries. This shows where arteries are blocked.
- The chances that problems will develop during cardiac cath are low.
A cardiac cath provides information on how well your heart works, identifies problems, and allows for procedures to open blocked arteries. For example, during cardiac cath your doctor may:
- Take X-rays using contrast dye injected through the catheter to look for narrowed or blocked coronary arteries. This is called coronary angiography or coronary arteriography.
- Perform a percutaneous coronary intervention (PCI) such as coronary angioplasty with stenting to open up narrowed or blocked segments of a coronary artery.
- Check the pressure in the four chambers of your heart.
- Take samples of blood to measure the oxygen content in the four chambers of your heart.
- Evaluate the ability of the pumping chambers to contract.
- Look for defects in the valves or chambers of your heart.
- Remove a small piece of heart tissue to examine under a microscope (biopsy).
Cardiac cath is usually very safe. A small number of people have minor problems. Some develop bruises where the catheter had been inserted (puncture site). The contrast dye that makes the arteries show up on X-rays causes some people to feel sick to their stomachs, get itchy, or develop hives.
- You will be given instructions about what to eat and drink during the 24 hours before the test.
- Tell your doctor about any medicines (including over-the-counter, herbs, and vitamins) you take. The doctor may ask you not to take them before your cath procedure. Don’t stop taking your medicine until your doctor tells you to.
- Tell your doctor or nurse if you are allergic to anything, especially iodine, shellfish, latex or rubber products, medicines like penicillin, or X-ray dye.
- Arrange to have someone drive you home after your procedure.
- If you usually wear a hearing aid, wear it during your procedure. If you wear glasses, bring them to your appointment.
- A doctor with special training performs the procedure with a team of nurses and other medical professionals. The procedure is done in a hospital cardiac catheterization (cath) lab.
Talk with your doctor. Here are some good questions to ask:
- What will you learn from the procedure?
- When will I get my results?
- When can I resume my normal activities?
- What medicines will I need to take?
- Will I need another treatment?
For more information, please contact our office at (586) 580-3062 for a consultation.
Percutaneous Coronary Intervention (PCI)
 Your heart’s arteries can become blocked or narrowed from a buildup of cholesterol, cells, or other substances (plaque). This can reduce blood flow to your heart and cause chest discomfort. Sometimes a blood clot can suddenly form or get worse and completely block blood flow, leading to a heart attack.
Your heart’s arteries can become blocked or narrowed from a buildup of cholesterol, cells, or other substances (plaque). This can reduce blood flow to your heart and cause chest discomfort. Sometimes a blood clot can suddenly form or get worse and completely block blood flow, leading to a heart attack.
Angioplasty opens blocked arteries and restores normal blood flow to your heart muscle. It is not major surgery. It is done by threading a catheter (thin tube) through a small puncture in a leg or arm artery to the heart. The blocked artery is opened by inflating a tiny balloon in it.
With coronary angioplasty, a thin, expandable balloon is inserted into the clogged artery and is inflated. This opens the artery by pushing the plaque against the artery wall. The balloon is then removed and blood flows more easily through the artery.
People with blockages in their heart arteries may need angioplasty if they are having lots of discomfort in their chest, or if their blockages put them at risk of a heart attack or of dying.
- A doctor numbs a spot on your groin or arm and inserts a small tube (catheter) into an artery.
- The catheter is threaded through the arterial system until it gets into a coronary (heart) artery.
- Watching on a special X-ray screen, the doctor moves the catheter into the artery. Next, a very thin wire is threaded through the catheter and across the blockage. Over this wire, a catheter with a thin, expandable balloon on the end is passed to the blockage.
- The balloon is inflated. It pushes plaque to the side and stretches the artery open, so blood can flow more easily. This may be done more than once.
- In many patients a collapsed wire mesh tube (stent) mounted on a special balloon is moved over the wire to the blocked area.
- As the balloon is inflated, it opens the stent against the artery walls. The stent locks in this position and helps keep the artery open.
- The balloon and catheters are taken out. Now the artery has been opened, and your heart will get the blood it needs.
No. Angioplasty causes very little pain. The doctor will numb the place where the catheter will be inserted. You may feel some pressure as the catheter is put in.
- You’ll be awake and alert but may be given medicine to help you relax.
- The place where the catheter was put in may be sore afterwards. Bruising is also common. If you notice any bleeding or increasing pain or swelling, tell your doctor.
- When the tube is removed from your leg or arm, a nurse or doctor will usually apply direct pressure for 15 minutes or longer to the place where the catheter was inserted to ensure there’s no internal bleeding.
- If angioplasty is done through the leg, for several hours you’ll lie quietly on your back, and the doctors and nurses will check for any signs of bleeding or chest discomfort. If the procedure is done through the arm, you won’t need to remain in bed.
- You’ll almost always have to stay in the hospital for a night to rest. Sometimes a longer stay is required.
- There’s a small risk that a blood clot will form inside the stent, blocking blood flow in the artery. Your doctor will prescribe aspirin or other medicine to help prevent this.
- Avoid heavy lifting or vigorous physical activity for 1-2 days after the procedure.
- Learn about the risk factors you need to change to keep your heart healthy.
Magnetic Resonance Angiography (MRA) or Imaging (MRI)
Magnetic Resonance Angiogram (MRA)
A magnetic resonance angiogram (MRA) is a type of magnetic resonance imaging (MRI) scan that uses a magnetic field and pulses of radio wave energy to provide pictures of blood vessels inside the body. In many cases MRA can provide information that can’t be obtained from an X-ray, ultrasound, or computed tomography (CT) scan.
MRA can find problems with the blood vessels that may be causing reduced blood flow. With MRA, both the blood flow and the condition of the blood vessel walls can be seen. The test is often used to look at the blood vessels that go to the brain, kidneys, and legs. Information from an MRA can be saved and stored on a computer for further study. Photographs of selected views can also be made.
During MRA, the area of the body being studied is placed inside an MRI machine. Contrast material is often used during MRA to make blood vessels show up more clearly.
A magnetic resonance angiogram (MRA) is done to look for:
- A bulge (aneurysm), clot, or the buildup of fat and calcium deposits (stenosis caused by plaque) in the blood vessels leading to the brain.
- An aneurysm or tear (dissection) in the aorta, which carries blood from the heart to the rest of the body.
- Narrowing (stenosis) of the blood vessels leading to the heart, lungs, kidneys, or legs.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a test that uses a magnetic field and pulses of radio wave energy to make pictures of organs and structures inside the body. In many cases MRI gives different information about structures in the body than can be seen with an X-ray, ultrasound, or computed tomography (CT) scan. MRI also may show problems that cannot be seen with other imaging methods.
For an MRI test, the area of the body being studied is placed inside a special machine that contains a strong magnet. Pictures from an MRI scan are digital images that can be saved and stored on a computer for more study. The images also can be reviewed remotely, such as in a clinic or an operating room. In some cases, contrast material may be used during the MRI scan to show certain structures more clearly.
You may be able to have an MRI with an open machine that doesn’t enclose your entire body. But open MRI machines aren’t available everywhere. The pictures from an open MRI may not be as good as those from a standard MRI machine.
Magnetic resonance imaging (MRI) is done for many reasons. It is used to find problems such as tumors, bleeding, injury, blood vessel diseases, or infection. MRI also may be done to provide more information about a problem seen on an X-ray, ultrasound scan, or CT scan. Contrast material may be used during MRI to show abnormal tissue more clearly. An MRI scan can be done for the:
- Head: MRI can look at the brain for tumors, an aneurysm, bleeding in the brain, nerve injury, and other problems, such as damage caused by a stroke. MRI can also find problems of the eyes and optic nerves, and the ears and auditory nerves.
- Chest: MRI of the chest can look at the heart, the valves, and coronary blood vessels. It can show if the heart or lungs are damaged. MRI of the chest may also be used to look for breast or lung cancer.
- Blood vessels: Using MRI to look at blood vessels and the flow of blood through them is called magnetic resonance angiography (MRA). It can find problems of the arteries and veins, such as an aneurysm, a blocked blood vessel, or the torn lining of a blood vessel (dissection). Sometimes contrast material is used to see the blood vessels more clearly.
There are no known harmful effects from the strong magnetic field used for MRI. But the magnet is very powerful. The magnet may affect pacemakers, artificial limbs, and other medical devices that contain iron. The magnet will stop a watch that is close to the magnet. Any loose metal object has the risk of causing damage or injury if it gets pulled toward the strong magnet.
Metal parts in the eyes can damage the retina. If you may have metal fragments in the eye, an X-ray of the eyes may be done before the MRI. If metal is found, the MRI will not be done.
Iron pigments in tattoos or tattooed eyeliner can cause skin or eye irritation.
An MRI can cause a burn with some medication patches. Be sure to tell your health professional if you are wearing a patch.
There is a slight risk of an allergic reaction if contrast material is used during the MRI. But most reactions are mild and can be treated using medicine. There also is a slight risk of an infection at the IV site.
Reasons you may not be able to have the test or why the results may not be helpful include:
- Pregnancy: An MRI test usually is not done during pregnancy. But MRI may be done to get more information about a possible problem that cannot be seen clearly with ultrasound.
- Medical devices that use electronics, such as a pacemaker or medicine infusion pump: The MRI magnet may cause problems with these devices, and that may keep you from having an MRI.
- Medical devices that have metal in them: The metal might make some of the detailed MRI pictures blurry. This may prevent your doctor from seeing the organ that is being looked at. For example, an intrauterine device (IUD) with metal may prevent your doctor from seeing the uterus clearly.
- Inability to remain still during the test.
- Obesity: A person who is very overweight may not fit into standard MRI machines.
Many modern medical devices that do not use electronics — such as heart valves, stents, or clips — can be safely placed in most MRI machines. But some newer MRI machines have stronger magnets. The safety of MRI scans with these stronger MRI magnets in people with medical devices is not known.
Cardiac Stable Ischemic Heart Disease
Ischemic heart disease means that the heart muscle is being deprived of the oxygen-rich blood it needs to function because of clogged coronary arteries.
More than 13 million people in the United States have coronary artery disease, and nearly 9 million have chest pain (angina).
If you have ischemic heart disease you may experience chest pain when you put extra demands on your heart, such as during exercise or stress. However, arm pain during exercise and shortness of breath are also symptoms of ischemia.
The right treatment for you will depend on how high-risk your heart disease is and other factors, such as your age, other medical conditions, and personal preferences. It is essential that you play an active role in learning about your condition and weighing the treatment options your doctor will discuss with you.
To get a clear understanding about your heart disease and begin to estimate your risk of serious complications such as a heart attack, your doctor may:
- Ask you questions about your chest pain and other heart-related symptoms, overall health, lifestyle, and family history.
- Order blood tests to check your cholesterol levels, blood sugar, kidney function, and several other important health indicators.
- Run a resting electrocardiogram (ECG or EKG) to check your heart’s rhythm and electrical system.
- Order a stress test to see how your heart responds when it is beating rapidly.
The stress test will help determine whether you have ischemic heart disease. It may also show what part and how large an area of heart muscle is being deprived of oxygen-rich blood. This will help determine how high your cardiac risk is. The type of stress test your doctor orders will depend on many things, including whether you can exercise strenuously and how high your cardiac risk is estimated to be before the test.
The most common option is ECG exercise stress testing, but your doctor may also order a stress test that uses echocardiography (ultrasound for the heart) or nuclear scanning. If you can’t exercise vigorously, your doctor will order a stress test that uses medication to make your heart beat faster, paired with echocardiography, nuclear scanning, or cardiac magnetic resonance imaging. Your doctor may also choose cardiac computed tomographic angiography (CCTA) to examine your heart and blood vessels.
- Order an imaging test — usually echocardiography — to be done while you rest quietly, to check your heart’s size and shape, how well it is pumping, and the motion of your heart valves. This resting test is usually done for patients who have previously had a heart attack, have signs of heart failure, have a complex arrhythmia, or a heart murmur. Resting tests may also be done using nuclear imaging.
- Refer you to an invasive cardiologist for cardiac catheterization (angiography). In this test, dye is injected into the arteries of your heart so that blockages can be seen on X-rays. This test is usually done only for patients who have high-risk results on their stress test, or have other high-risk problems such as cardiac arrest, a serious disturbance in the heart’s rhythm, or signs of heart failure.
To keep you healthy, your doctor may recommend:
- Participation in a cardiac rehabilitation program, to support you in making healthy lifestyle changes and in managing medications.
- A non-invasive therapy called enhanced external counter pulsation may also be used to relieve chest pain in certain patients. However, this therapy is not recommended for certain patients, including those with peripheral artery disease, severe heart failure, and severe aortic regurgitation.
- A procedure to restore good blood flow to your heart. This may be necessary if the build-up of cholesterol plaque (atherosclerosis) is causing severe and dangerous blockages in your arteries, or if medication alone is not enough to control your symptoms.
The choice typically is between open-chest coronary artery bypass graft surgery (CABG) and minimally invasive percutaneous coronary intervention (PCI, also called angioplasty and stenting). CABG is recommended over PCI in patients with diabetes and complex multivessel disease and in some patients, doctors may use a “hybrid” combination of the two procedures to improve blood flow to the heart. The best approach will depend on where the blockages are, how severe they are, how many arteries are involved, and your overall health.
Healthy lifestyle habits that include:
- Eating a diet that is low in cholesterol, saturated fats, trans fats, and salt, and that includes lots of fresh fruits and vegetables and whole grains.
- Maintaining a healthy body weight.
- Exercising 30 to 60 minutes at moderate intensity, such as brisk walking, at least 5 days a week.
- Taking steps to reduce stress and relieve depression.
- Stopping smoking and avoiding secondhand smoke.
- Limiting alcohol intake to 1 to 2 drinks a day for men and 1 drink a day for women.
- Getting an annual flu shot.
Medications that:
- Keep blood levels of cholesterol and other lipids under control (usually statins).
- Keep blood pressure under good control.
- Prevent heart attack, including daily low-dose aspirin (75 to 162 mg), clopidogrel (Plavix) if you are at high risk, beta blockers, and angiotensin-converting-enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs).
- Relieve chest pain and other symptoms, including beta blockers and nitroglycerin tablets to put under your tongue in case you suddenly develop chest pain. Some patients may need calcium-channel blockers or long-acting nitrates instead.
- Achieve good diabetes control, including keeping the hemoglobin A1c at rec goal.
Your doctor and heart care team will present all your options, and you will play a key role in making this important decision. This heart care team typically includes an interventional cardiologist and a cardiac surgeon who work with you to review your medical history and health status, discuss possible treatment options, and select the best treatment strategy for you.
To help you stay healthy over the long run, your doctor may:
- Talk to you about your symptoms and ability to participate in daily activities.
- Watch for any complications, including heart failure or arrhythmias.
- Keep an eye on risk factors, such as cholesterol levels, blood pressure, and diabetes control.
- Encourage you to continue healthy lifestyle changes.
- Make sure you are following your medication plan.
- Order a stress test if you are having problems with new or worsening symptoms, such as chest pain or shortness of breath.
For more information, please contact our office at (586) 580-3062 for a consultation.
Balloon (Angioplasty)
Angioplasty is a procedure done to open a partially blocked blood vessel so that blood can flow through it more easily. It is most often done on arteries that deliver blood to the heart (coronary arteries) when they are narrowed by plaque buildup (atherosclerosis) or blood clots.
During the angioplasty procedure, a thin flexible tube (catheter) is inserted through an artery in the groin, arm, or wrist and is carefully guided into the artery that is narrowed. After the tube reaches the narrowed artery, a small balloon at the end of the tube is inflated. The balloon may remain inflated for a short time. The pressure from the inflated balloon presses fat and calcium deposits (plaque) against the wall of the artery to improve blood flow.
Angioplasty gets blood flowing back to the heart. It opens a coronary artery that was narrowed or blocked during a heart attack. The coronary artery might be blocked by a blood clot and fat and calcium from a ruptured plaque that caused the heart attack.
Doctors try to do angioplasty as soon as possible after a heart attack. Angioplasty is not available in all hospitals. If a person is at a hospital that does not do angioplasty, he or she might be moved to another hospital where angioplasty can be done.
Angioplasty is also called percutaneous coronary intervention (PCI) or percutaneous transluminal coronary angioplasty (PTCA).
Angioplasty is done using a thin, soft tube called a catheter. A doctor inserts the catheter into a blood vessel in the groin or wrist. The doctor carefully guides the catheter through blood vessels until it reaches coronary arteries on the heart.
- Cardiac catheterization, also called coronary angiogram: Your doctor first uses the catheter to find narrowing or blockages in the coronary arteries. This is done by injecting a dye that contains iodine into the arteries. The dye makes the coronary arteries visible on a digital X-ray screen. This testing is also called a coronary angiogram.
- Balloon with or without a stent. If there is a blockage, the catheter is moved to the narrowed part of the artery. A tiny balloon is moved through the catheter and is used to open the artery. The balloon is inflated for a short time. Then it is deflated and removed. The pressure from the inflated balloon makes more room for the blood to flow because the balloon presses the plaque against the wall of the artery. The doctor can also use the balloon to place a stent in the artery to keep it open.
In some cases, the doctor might remove loose pieces of blood clots from the artery. This is done with a small device that is like a vacuum. The doctor moves the device up through the catheter to the blocked artery and removes the clot pieces. This is a newer procedure that can be used during angioplasty.
After angioplasty, you will be moved to a recovery room or to the coronary care unit. Your heart rate, pulse, and blood pressure will be closely watched. You will have a large bandage or a compression device at the catheter insertion site to prevent bleeding.
An angioplasty may take 30 to 90 minutes. But you need time to get ready for it and time to recover. It can take several hours total.
People usually can start walking in 12 to 24 hours after angioplasty. The average hospital stay is 1 to 2 days for uncomplicated procedures. You may resume exercise and driving after several days.
After angioplasty, you will take antiplatelet medicines to help prevent another heart attack or a stroke. You will probably take aspirin plus another antiplatelet such as clopidogrel (Plavix). If you get a drug-eluting stent, you will probably take both of these medicines for at least one year. If you get a bare metal stent, you will take both medicines for at least one month but maybe up to one year. Then you will likely take daily aspirin long-term. If you have a high risk of bleeding, your doctor may shorten the time you take these medicines.
After your procedure, you might attend a cardiac rehabilitation program. In cardiac rehab, a team of health professionals provides education and support to help you recover and start new, healthy habits, such as eating right and getting more exercise. To keep your heart healthy and your arteries open, making these changes is just as important as getting treatment.
Emergency angioplasty with or without stenting is typically the first choice of treatment for a heart attack.
Although many things are involved, angioplasty might be done if you:
- Are having a heart attack.
- Have frequent or severe angina that is not responding to medicine and lifestyle changes.
- Have evidence of severely reduced blood flow (ischemia) to an area of heart muscle caused by one or more narrowed coronary arteries.
- Have a narrowed or blocked artery that is likely to be treated successfully with angioplasty.
- Are in good enough health to have the procedure.
Angioplasty might not be a reasonable treatment option when:
- There is no evidence of reduced blood flow to the heart muscle.
- Only small areas of the heart are at risk, and you do not have disabling angina symptoms.
- You are at risk for having complications or dying during angioplasty due to other health problems.
- You cannot take blood thinner medicines, aspirin, or any other antiplatelet after getting a stent.
- The affected artery cannot be reached during angioplasty.
For more information, please contact our office at (586) 580-3062 for a consultation.
Stent
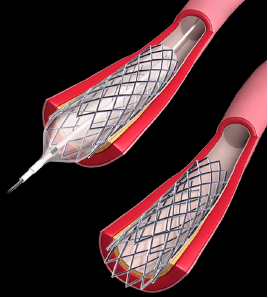 A stent is a tiny wire mesh tube. It props open an artery and is left there permanently. When a coronary artery (an artery feeding the heart muscle) is narrowed by a buildup of fatty deposits called plaque, it can reduce blood flow. If blood flow to the heart muscle is reduced, chest pain can result. If a clot forms and completely blocks the blood flow to part of the heart muscle, a heart attack results.
A stent is a tiny wire mesh tube. It props open an artery and is left there permanently. When a coronary artery (an artery feeding the heart muscle) is narrowed by a buildup of fatty deposits called plaque, it can reduce blood flow. If blood flow to the heart muscle is reduced, chest pain can result. If a clot forms and completely blocks the blood flow to part of the heart muscle, a heart attack results.
Stents help keep coronary arteries open and reduce the chance of a heart attack.
A stent is inserted into the clogged artery with a balloon catheter. The balloon is inflated, and the stent expands and locks in place. This holds the artery open and allows blood to flow more freely.
To open a narrowed artery, a doctor may do a procedure called a percutaneous coronary intervention (PCI) or angioplasty. In it, a balloon-tipped tube (catheter) is inserted into an artery and moved to the point of blockage. Then the balloon is inflated. This compresses the plaque and opens the narrowed spot. When the opening in the vessel has been widened, the balloon is deflated and the catheter is withdrawn.
When a stent is used, it’s collapsed and put over the balloon catheter. It’s then moved into the area of the blockage. When the balloon is inflated, the stent expands, locks in place, and forms a scaffold. This holds the artery open. The stent stays in the artery permanently and holds it open. This improves blood flow to the heart muscle and relieves symptoms (usually chest pain).
Stents are used depending on certain features of the artery blockage. Factors that affect whether a stent can be used include the size of the artery and where the blockage is. Stenting has become fairly common. Most angioplasty procedures are done using stents.
In certain patients, stents reduce the renarrowing that sometimes occurs after balloon angioplasty or other procedures that use catheters.
Patients who have angioplasty and stents recover from these procedures much faster than patients who have coronary artery bypass surgery (CABG). They have much less discomfort, too.
In over a third of patients who’ve had angioplasty without a stent, the artery that was opened begins to become narrowed again within months of the procedure. This renarrowing is called restenosis.
Stents help prevent this. There are two types of stents. Stents that are covered with drugs that help keep the blood vessel from reclosing are called drug-eluting stents. Stents not coated with drugs are called bare metal stents. If stents don’t work and the arteries reclose, you may need coronary artery bypass surgery (CABG).
You will need to take one or more antiplatelet agents. These medicines keep platelets from clumping together and forming blood clots in the stent and blocking the artery.
One antiplatelet agent is aspirin. A second type is called a P2Y12 inhibitor. You may be prescribed one of three P2Y12 inhibitors: — clopidogrel, prasugrel, or ticagrelor. Which one of these medications your doctor prescribes will be based on what he or she feels is best for you, based on your risk of blood clots and bleeding. When aspirin and a P2Y12 inhibitor are used together, it is called dual antiplatelet therapy (DAPT).
In addition to DAPT, you may be prescribed additional medications as well.
Aspirin is used indefinitely. How long you need to take a P2Y12 inhibitor depends on why you are being prescribed the drug, as well as your future risk of blood clots and bleeding.
- If you had a heart attack, the general recommendation is that you should be on a P2Y12 inhibitor for at least a year. If you don’t have a high bleeding risk, longer duration of therapy may be beneficial and lower your risk of future heart attack.
- If you are a high bleeding risk, you may have been treated with a bare metal stent. In this case, you should take a P2Y12 inhibitor for at least one month.
- If you were treated with a drug-eluting stent, in general, you will be treated for at least 6-12 months with a P2Y12 inhibitor. If you are at a higher bleeding risk, you may be treated for a shorter period of time (3-6 months). If you don’t have a high bleeding risk, longer duration of therapy (more than 6-12 months) may be beneficial and lead to a lower risk of future heart attack and clotting of the stent.
It is important for you to take your medication as prescribed. Stopping it on your own can lead to a marked increase in risk of clots forming inside the stent, particularly in the first month or months after stent placement.